


Basal cell carcinoma (BCC) is the most common skin cancer worldwide, comprising about 75-80% of all new skin cancers diagnosed. The primary risk factor for developing BCC is UV exposure. Also, individuals with lighter skin tone, eye color, and/or hair color are at increased risk. Other additional risk factors include chronic arsenic exposure, radiation therapy, and inherited disorders, such as basal cell nevus syndrome, xeroderma pigmentosum, and albinism. It can be developed from nonhealing wounds. Even though it rarely metastasizes, it may cause significant morbidity if left untreated.
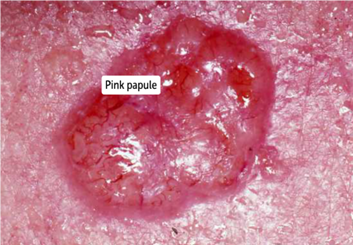
Basal cell carcinoma is typically found in sun-exposed areas, mainly the face, neck, and upper lip. BCC is frequently slow-growing and commonly appears as a pink, pearly papule or plaque with dilated vessels and rolled borders and is often painless (figure 1). A characteristic feature of BCC is dilated blood vessels, called telangiectasia. The diagnosis of BCC is made by a dermatologist through a skin biopsy. For this reason, since dermatologists are specialists trained to perform skin biopsies and evaluate skin lesions, it is essential to consult one for suspicious skin lesions.
1. Squamous cell carcinoma
Squamous cell carcinoma (SCC) is the second most common skin cancer. The primary risk factor for SCC is cumulative sun exposure (either from sun or tanning beds). Chronic immunosuppression, chronic non-healing wounds, arsenic exposure, ionizing radiation, and light skin tone individuals are other risk factors. Typically appears on face, lower lips, ears, and hands. SCC tends to grow faster than BCC.
Different from basal cell carcinoma, squamous cell carcinoma has a premalignant lesion, called actinic keratosis. This premalignant lesion is caused by sun exposure and is described as small, rough, erythematous or brownish papule or plaque or as a cutaneous horn (figure 2).


2. Melanoma

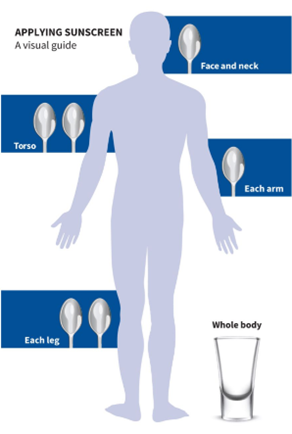
These recommendations apply to all fair-skinned individuals, outdoor workers, children, and people at high risk of skin cancer.
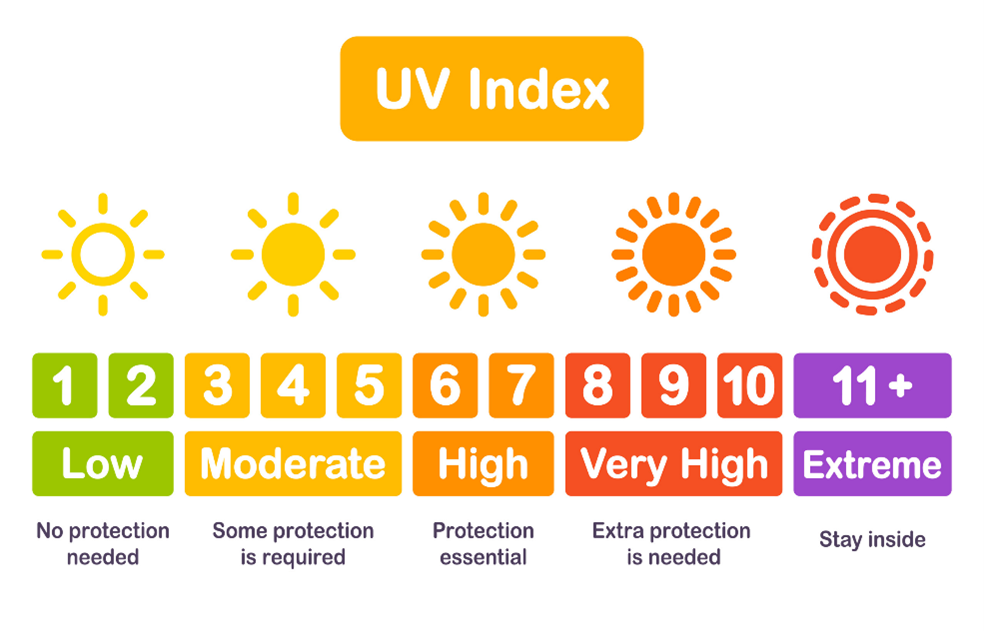
Finally, we cannot leave this blog without talking about the different types of UV radiation. There are 3 main types of UV rays that the sun is emitting right now: UVA, UVB, and UVC. Almost all the UV radiation reaching the earth is UVA rays, accounting 95% to be precise, which is the main cause of photoaging due to their ability to penetrate deeper into the skin. UVA rays induce DNA damage mediated by the formation of free radicals via reactive oxygen species and decrease the activity of antigen-presenting cells of the epidermis. On the contrary, UVB rays are known as sunburn rays and are more classically associated with skin cancer than UVA tanning rays. UVB radiation induces DNA lesions forming pyrimidine cross-links, such as pyrimidine dimers, between neighboring DNA base pairs. Finally, the third type of rays, the UVC rays, although more damaging to the skin than UVA and UVB, are completely absorbed by the ozone layer, and therefore, they do not increase the risk of skin cancer.